Galaxy Quality Suite
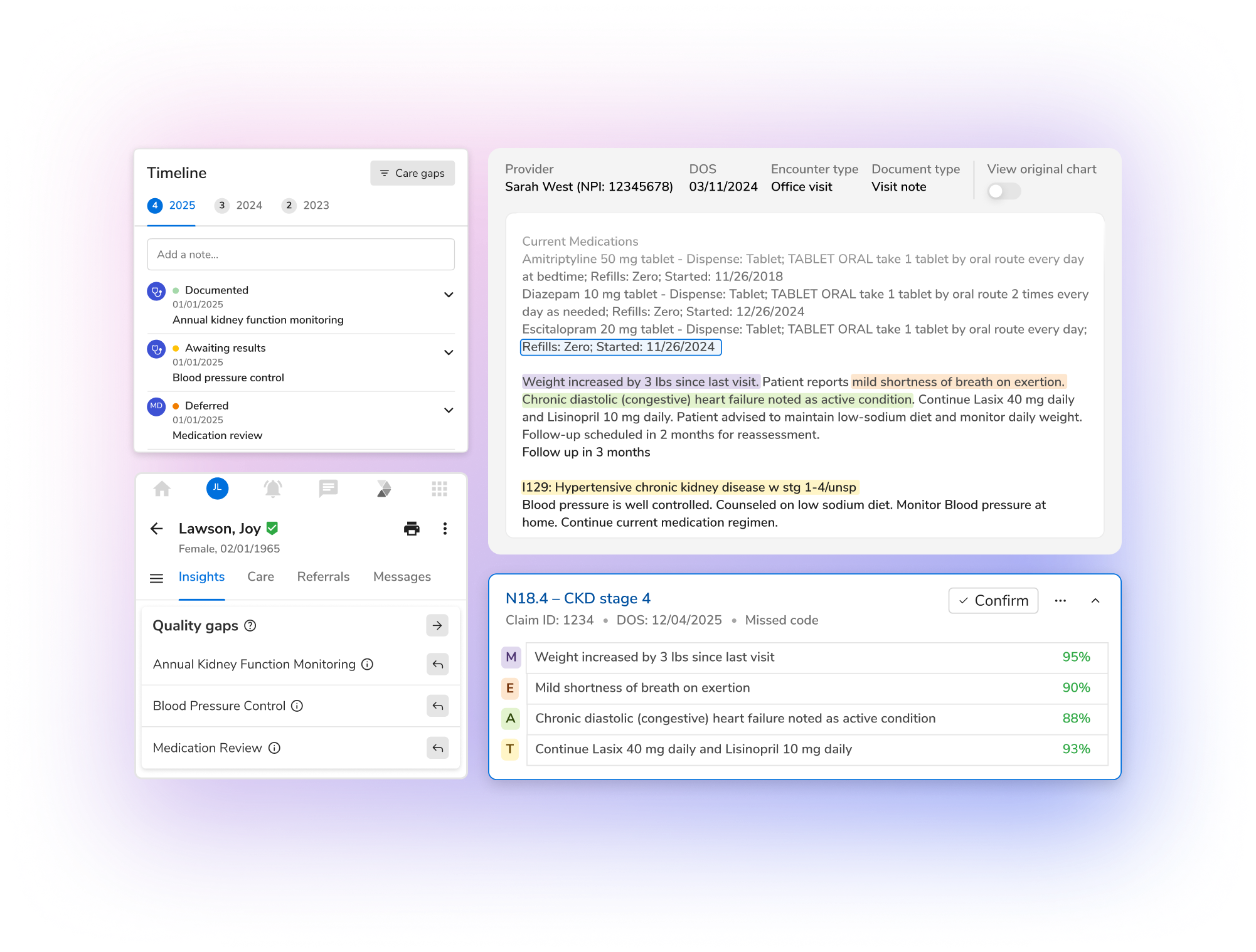
AI-powered quality management for proactive gap closure, greater efficiency, and audit-ready compliance.
Close care gaps faster, enhance Stars and HEDIS performance, and reduce manual effort with AI that unifies data, automates reviews, and drives measurable quality outcomes across every member touchpoint.
.avif)







.svg)