How Health Plans Can Improve Star Ratings Through Multipoint Gap Closure


In Houston, Texas, Dr. Jane R. Montealegre unfolded a troubling reality of cervical cancer: despite the proven effectiveness of cervical cancer screening, many women have never been screened or were overdue. To tackle this, her team enrolled nearly 2,500 women and divided them into three groups. The aim was to test whether at-home self-collection kits could improve cervical cancer screening rates. Group A received a call from a patient navigator to explain the importance of cervical cancer screening and invite them to get clinic-based screening. Her team at MD Anderson Cancer Center found that only 17% showed up within six months. The barriers were real: work schedules, childcare, transportation, and anxiety about clinical settings
Adopting a different approach with Group B, they mailed self-collection kits directly to their homes. The results were striking: 41% completed their screening, 2.4 times more than those who'd only received a phone call. In Group C, women received both a kit and personalized follow-up support to guide them through the process; the number climbed even higher to 47%.
In another study, it was found that pharmacy intervention was linked to nearly a threefold increase in the likelihood of closing care gaps. This highlights the role pharmacies can play in identifying and prompting closure of care gaps, contributing significantly to improved patient outcomes and plan performance.
Together, these insights confirm that a one-way approach to closing care gaps is not efficient anymore. The need is to connect multiple doorways to reach members, overcome barriers, and improve health outcomes comprehensively.
The Solution: Multipoint Gap Closure
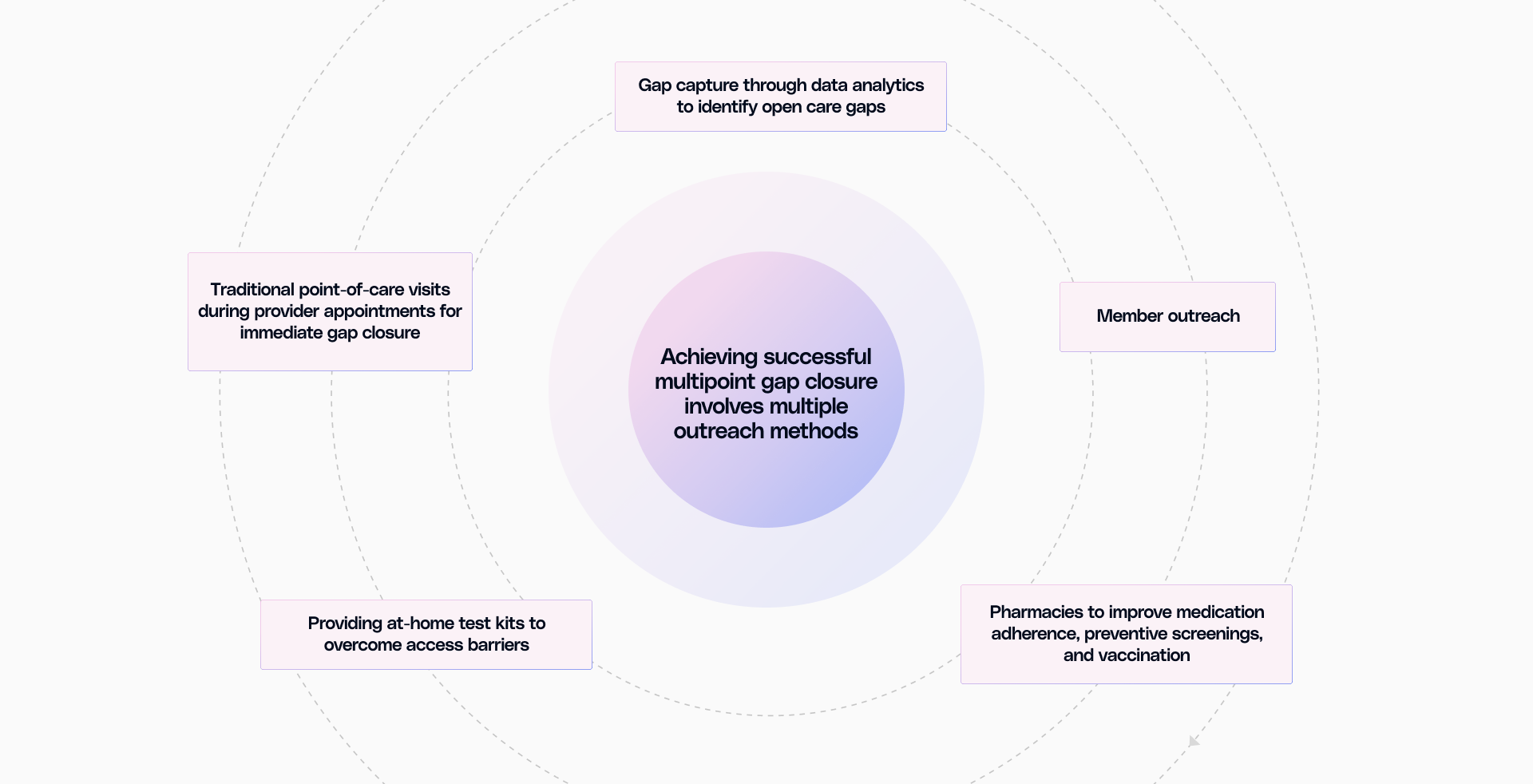
When health plans reach out through only one channel, gaps often remain open. This is where the need for multipoint gap closure arises. It uses pharmacy interventions, member outreach, home test kits, and point-of-care prompts so that the next interaction with a provider, pharmacy, or even at home can result in a closed gap. What powers all of this is the unification of disparate data sources, such as claims, clinical records, labs, and pharmacy data, to get a full picture of each member’s needs and opportunities.
Plans with open gaps often see lower Star ratings and overall plan performance. With multipoint gap closure, payers maintain high performance and capture incentives more consistently.
Operational efficiency is another direct benefit. Instead of engaging the same members with the same outreach for each overdue service, multipoint gap closure lets teams act quickly through a unified platform. For example, for a member with diabetes who has missed their HbA1c, the Stars dashboard highlights the gap; the plan can nudge the member for a provider visit, send a prompt through our provider engagement tool so their physician is reminded to check for blood sugar during the next visit, and notify the pharmacy to do so as well. If the member goes to either location, the reading can be recorded, closing the gap and improving chances of a better Star rating. If this still doesn’t work, an at-home test kit can be sent with just one click to capture the gap effectively.
This approach creates a smarter intervention, too. Some members require education about the importance of screening, some face problems like a lack of transportation, and others just benefit from reminders. Galaxy’s multipoint gap closure platform enables you to select the outreach most likely to generate results. This ensures plans deliver the right action at the right time, through the best channel for each person.
Focused resources are achieved through real-time analytics, helping quality teams track which gaps are being resolved and which outreach methods work best. Staff time moves from troubleshooting data errors or generic reminder calls to addressing genuine barriers and delivering meaningful outcomes.
What Star Ratings Mean for Health Plans
The Centers for Medicare & Medicaid Services (CMS) uses the Star Ratings program to measure Medicare Advantage and Prescription Drug plan performance. Plans earn one to five stars based on health outcomes, patient experience, chronic condition management, and preventive services. CMS assesses these areas through over 40 quality measures, which directly influence the plan’s reputation.
An Improved Star performance lifts three key areas for plans: incentives from CMS, new member enrollment, and existing member retention. When more gaps are closed, especially for chronic illness measures, data visibility and care outcomes rise across multiple Star categories. Members receive outreach that matches their needs and experience fewer redundant reminders, increasing satisfaction. Providers receive accurate gap lists, know which actions matter for Star results, and can focus on care rather than correcting data.
Traditional gap closure misses gaps that may already be resolved or occurred in settings other than the provider's office. Staff often waste valuable time, and members become frustrated with repeated outreach. As CMS continues tightening standards and expectations for reporting and outcomes, plans using one-dimensional gap closure strategies fall behind.
Making Multipoint Gap Closure Work
The success of multipoint gap closure hinges on robust technology and unified data. Galaxy aggregates relevant data into one patient record, enabling quality teams to track gaps across sources without jumping between systems. The gap closure module focuses interventions directly on Star measures; the intervention engine leverages this unified data to personalize outreach, whether at home, through pharmacies, or with providers.
Normalization and interoperability of data are paramount. Plans need to integrate feeds from labs, providers, pharmacies, and other sources. Uniform, integrated data allows for automated gap capture, efficient outreach, and continuous improvement. Outreach needs segmentation of members for strategizing interventions. Provider trust increases with more accurate gap lists, reducing alert fatigue and increasing participation.
The plan should monitor member satisfaction with the outreach, gap closure rates, and provider engagement to measure success.
Connect data and technology with Galaxy, and see Star ratings improve while members get better experiences. That's how payers should operate.
Ready to see this transformation in action?


.png)



.png)



.avif)









.svg)
.svg)

.svg)

